Navigating health insurance often feels like stepping into a maze of outdated processes and inefficient systems. Accessing vital information or filing a claim can seem nearly impossible for many.
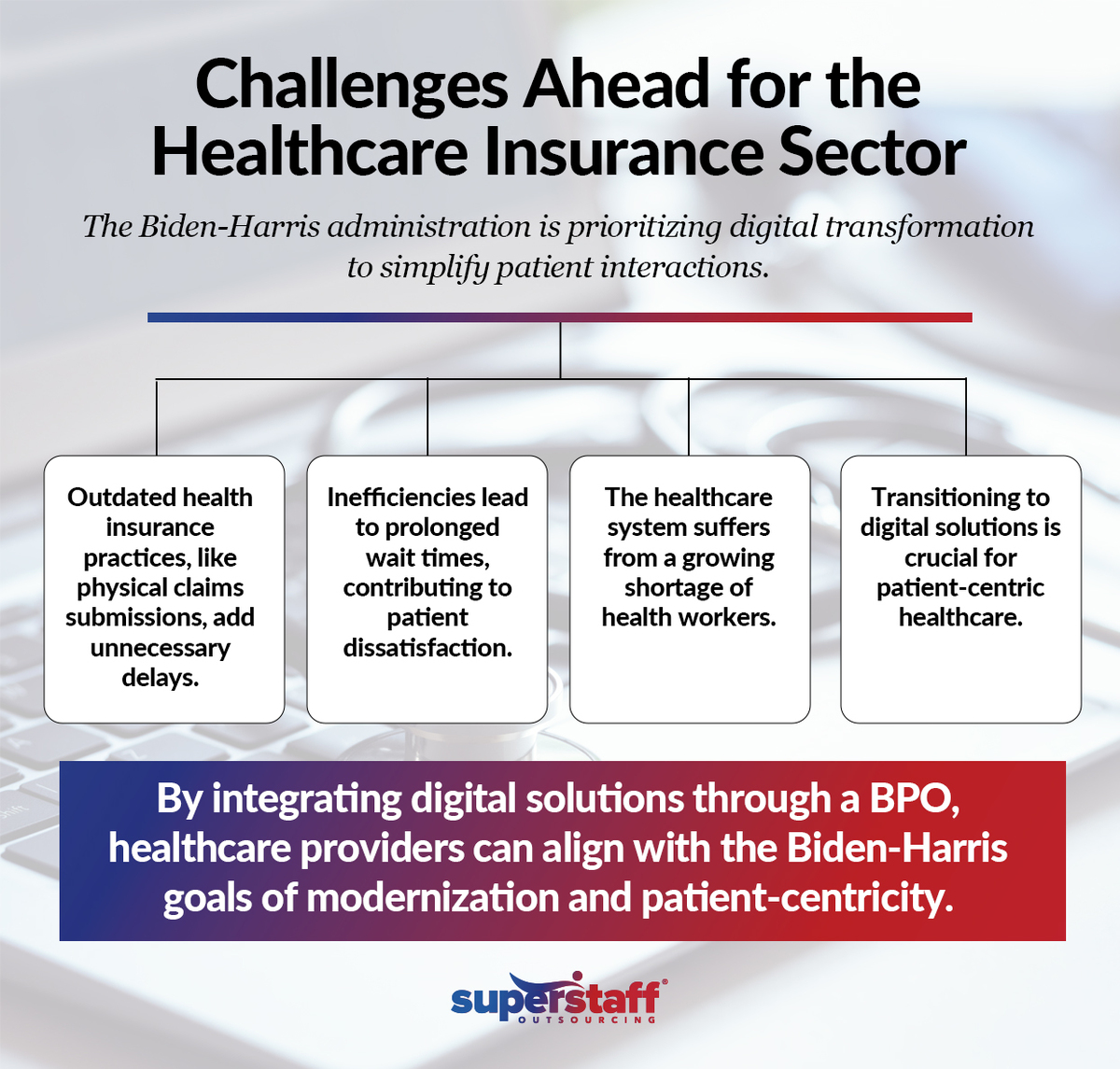
Despite technological advances, some of the most extensive health plans still require patients to print and physically mail claim forms — yes, in 2024. Meanwhile, clunky websites, long call center wait times, and restricted customer service hours add to the frustration, leaving patients stressed and inconvenienced.
Recognizing these growing pain points, the Departments of Health and Human Services (HHS) and Labor (DOL) are pushing health insurers and group plans to adopt solutions that save both time and money. These agencies champion patient-first reforms as part of the Biden administration’s “Time Is Money” initiative.
In the coming months, the Office of Personnel Management will mandate that Federal Employees Health Benefits and Postal Service Health Benefits plans — covering eight million Americans — modernize their systems. These changes will allow consumers to submit out-of-network claims online, easily access in-network provider details, and understand the steps to appeal claim denials. The goal? To simplify healthcare processes and make them more transparent and patient-centric.
Let’s examine this closely to see what it could mean for your business and how it may transform the healthcare landscape toward a patient-centric healthcare once again.
The Problem With the Current Health Insurance System
As health systems emerge from the COVID-19 pandemic, they face a landscape marked by significant financial and operational pressures. The industry’s challenges are particularly evident in the health insurance system, a quicksand for patients where every step forward is met with resistance. The processes that are supposed to protect and assist them are instead riddled with inefficiencies that waste valuable time and add unnecessary stress to an already complex experience.
At the heart of this issue is the outdated requirement that many health plans still impose on their customers: the need to print, scan, or physically mail health claims. In an era where digital solutions are the norm, this reliance on dated methods is inconvenient and reflects a broader lack of modernization within the healthcare industry. These outdated practices force patients to interrupt their daily lives, whether by taking time off work to visit a post office or spending hours on hold with customer service, all while trying to manage their health concerns.
The Hidden Costs of Inefficiency: Prolonged Wait Times and Limited Access
Imagine needing urgent help with your health insurance only to find yourself stuck on hold for an eternity. This grim reality is all too common and is one of the most glaring inefficiencies in the current healthcare system. You’re often met with confusing or outdated information even when you turn to online resources for quicker answers.
Adding to the problem is the growing shortage of health workers, which could leave us with a 10-20% gap in direct patient care. With fewer nurses (200,000 to 450,000 nurses by 2025) to handle patient needs and keep the system running smoothly, things have worsened — longer wait times and a considerable drop in the quality of care.
As a result, about 45% of Americans recently had to skip treatment or medicine due to cost or lack of access, painting a picture of how systemic inefficiencies are contributing to widespread frustration and difficulty.
These inefficiencies don’t just waste time — they erode trust. When patients can’t get the help they need promptly, whether due to long wait times or confusing online tools, the entire system feels like it’s working against them. This is particularly troubling given that 89.1% of adults aged 18 to 64 in the U.S. had health insurance in 2023, indicating that most citizens are navigating this complex and often ineffective system.
A Reliance on Outdated Methods
The health insurance system’s stubborn reliance on outdated methods—such as requiring physical forms and documents—creates unnecessary roadblocks for patients. In an age when nearly every other industry has embraced digital transformation, the healthcare system’s failure to do so is a glaring oversight.
For instance, many health plans still require customers to physically mail in their claims or forms, which is inconvenient and time-consuming. This leads to delays in processing and, ultimately, in receiving care. Roughly 41% of adults have reported debt from unpaid medical or dental bills, showing the grave financial impact of these inefficiencies.
These outdated practices are part of what experts call ‘doom loops’ — self-perpetuating cycles of inefficiency that prevent patients from receiving timely and effective healthcare. Each obstacle, whether a long wait time or a confusing website, burdens patients, making it harder for them to get the care they need when needed.
Transitioning to a Patient-Centric Healthcare Approach in Healthcare
Recognizing these systemic flaws, the Departments of Health and Human Services (HHS) and Labor (DOL) are taking steps to address these issues and break the cycle of doom loops. By pushing for digital modernization and advocating for more accessible and efficient healthcare processes, they aim to create a system that truly puts patients first.
In the coming months, new regulations and initiatives will be rolled out to ensure that health insurance companies and group health plans adopt digital solutions that make it easier for patients to manage their healthcare. These changes are designed to save patients time and money, reduce frustration, and ultimately improve the healthcare experience. Given that the average healthcare expenditure per capita in the U.S. is $12,555 — significantly higher than in other developed nations — embracing digital solutions and eliminating outdated practices is essential for moving the healthcare system closer to delivering the quality care patients deserve.
The transition to a more patient-centric healthcare system will not happen overnight. Still, today’s steps lay the groundwork for a future where healthcare is more accessible, efficient, and responsive to patients’ needs.
The Biden-Harris Administration’s Response
The Biden-Harris administration is taking a major initiative to modernize and simplify the healthcare experience. This move is about fixing systemic flaws, streamlining processes, and putting patients back at the heart of healthcare.
Tackling Inefficiencies Head-On
The Departments of Health and Human Services (HHS) and Labor (DOL) are leading the charge in this overhaul. Under the guidance of HHS Secretary Xavier Becerra and DOL Acting Secretary Julie Su, there’s a big push for digital transformation. The spotlight is on digital claims submission—moving away from the old, cumbersome paper-based system to a more efficient online process.
Simplifying Patient Interactions
The Biden-Harris administration’s new initiative is set to make interactions with health insurance plans much easier for patients. Instead of dealing with confusing paperwork and waiting endlessly on hold, this effort aims to clear up the clutter. The push is for insurers to provide straightforward information, cutting through the jargon and simplifying processes.
The goal is to transform the patient experience from a complex and stressful ordeal to something much smoother and more manageable. Streamlining these interactions helps your patients navigate insurance with less hassle and frustration.
Enhancing Digital Processes for Federal Employees
The new initiative’s big focus is improving digital processes for Federal Employees Health Benefits (FEHB) and Postal Service Health Benefits plans, which cover over 8 million Americans. The administration is pushing for significant updates to make things easier for everyone involved.
For instance, federal employees can soon submit out-of-network claims online, ditching those old, cumbersome paper forms. The updates also include more explicit and accessible information about in-network providers. Plus, if a claim gets denied, the appeal process will be simplified, reducing the stress and confusion that often accompany it. This overhaul aims to make managing health insurance claims and information much smoother and more user-friendly for your patients.
Restoring Patient-Centricity in Healthcare
The initiative isn’t just about making things a bit easier; it’s about fundamentally refocusing on what matters — your patients. This effort is about ensuring the healthcare system truly serves the people it’s meant to protect. By tackling those deep-rooted inefficiencies that have been frustrating patients for too long, the administration is working to build a healthcare model that puts patient needs front and center.
This shift is part of a broader movement to restore trust in the healthcare system. It’s about cutting through the red tape and removing the barriers that have led to widespread dissatisfaction. The goal is to make healthcare not only more efficient and accessible but also more compassionate and responsive. As this initiative moves forward, there’s real hope that it will lead to a future where healthcare is streamlined, patient-focused, and genuinely effective in meeting the needs of those it serves.
How Online Claim Submissions Benefit Your Patients
Allowing patients to submit health claims online is a game-changer for your healthcare business, especially if outdated manual methods still bog down your current processes. This shift to digital submissions isn’t just a technological upgrade; it’s a significant enhancement in patient experience.
Streamlining the claims process and minimizing administrative headaches will offer your patients a smoother, more efficient service.
24/7 Access to Submissions
Gone are the days of being tethered to restrictive call center hours or scrambling to complete paperwork within the confines of a 9-to-5 schedule. With digital platforms, patients can submit their claims anytime that suits them best — whether late at night, early in the morning, or even during the weekend.
Before digital submissions, patients might have been forced to take time off work or wait for an opportunity to call during business hours, creating stress and potential delays. Now, they can simply log in to the online portal at their convenience, upload their documents, and complete their claims without the pressure of fitting into a specific time window.
This level of accessibility doesn’t just simplify things for your patients; it significantly reduces their stress and frustration. When patients are no longer constrained by limited service hours, they feel more in control of their healthcare management. This flexibility leads to a smoother, more satisfying experience and can ultimately enhance their overall perception of your services.
Real-Time Tracking and Information Access
With digital systems, patients can get instant updates and check their claim’s progress anytime.
Imagine the frustration of waiting for weeks, unsure if their claim has been processed or if there’s a problem. This uncertainty can create a lot of anxiety for your patients. But with real-time tracking, they can see precisely where their claim stands at any given moment. Whether they’re checking on their lunch break, late at night, or during a quiet day, your patients will have immediate access to their claim status.
This level of transparency eases anxiety and keeps your patients feeling informed and in control throughout the process. By providing real-time updates, you’re enhancing their experience with your services and building trust. It’s a simple yet powerful way to show that you value their peace of mind and are committed to a smooth, efficient claims process.
Reduced Risk of Lost Documents
Let’s dive into the benefits of digital document management. In a conventional filing system, paperwork can go missing, leading to delays and frustration. You can put those worries to rest with a fully automated system.
All your records are securely stored and organized in one place. This significantly reduces the chances of documents getting lost or misplaced. Fewer lost documents mean faster processing times and quicker reimbursements, which helps streamline your operations.
This translates into fewer administrative headaches for your team. No more sifting through piles of paper or tracking down missing forms. Everything is neatly archived and easily accessible, allowing your team to focus on what truly matters—providing excellent service and managing patient needs.
Beyond Convenience and Efficiency
The shift to online claim submissions is a game-changer for how you interact with your patients. When you modernize how health claims are handled, you do more than just speed up processes. You’re fundamentally transforming the patient experience. By adopting digital solutions, you’re meeting patient needs with better speed and accuracy — showing that you’re committed to reliability and modern care.
This move helps rebuild trust and sets a new standard for patient satisfaction. It demonstrates that you’re not just keeping up with the times but leading the way in delivering a top-notch, patient-focused experience. So, while the improvements in convenience and efficiency are significant, they’re just the start of a broader transformation in how your business engages with and supports your patients.
Toward a Fully Patient-Centric Healthcare System
Moving to online claims submission is a big step toward staying ahead of healthcare trends and making healthcare genuinely patient-focused. It’s about ditching outdated processes and putting patients’ needs front and center.
Here’s how this shift is making a difference:
Transparency in Provider Networks and Claim Denials
Studies show that 80% of patients prefer digital communication with their healthcare providers.
They want to know which providers are in-network and how to handle claim denials without getting lost in the system. Clear, straightforward information helps them make better choices and avoids unexpected costs. Making this info easy to find and understand reduces confusion and improves the overall experience.
Easy-to-Understand Coverage Information
Patients must also know what their coverage entails without wading through complicated jargon. With 44% of them expecting proactive communication from their providers, they want more engagement. When you provide clear and straightforward information, patients can interact with their healthcare providers more effectively, leading to better health outcomes.
A Unified Digital Experience
Did you know that 66% of consumers would choose a provider based on their ability to communicate in real-time? Streamlining these processes makes it easier for patients to interact with your services and reduces their frustration. The goal is to create a seamless digital experience that covers everything from booking appointments to submitting claims.
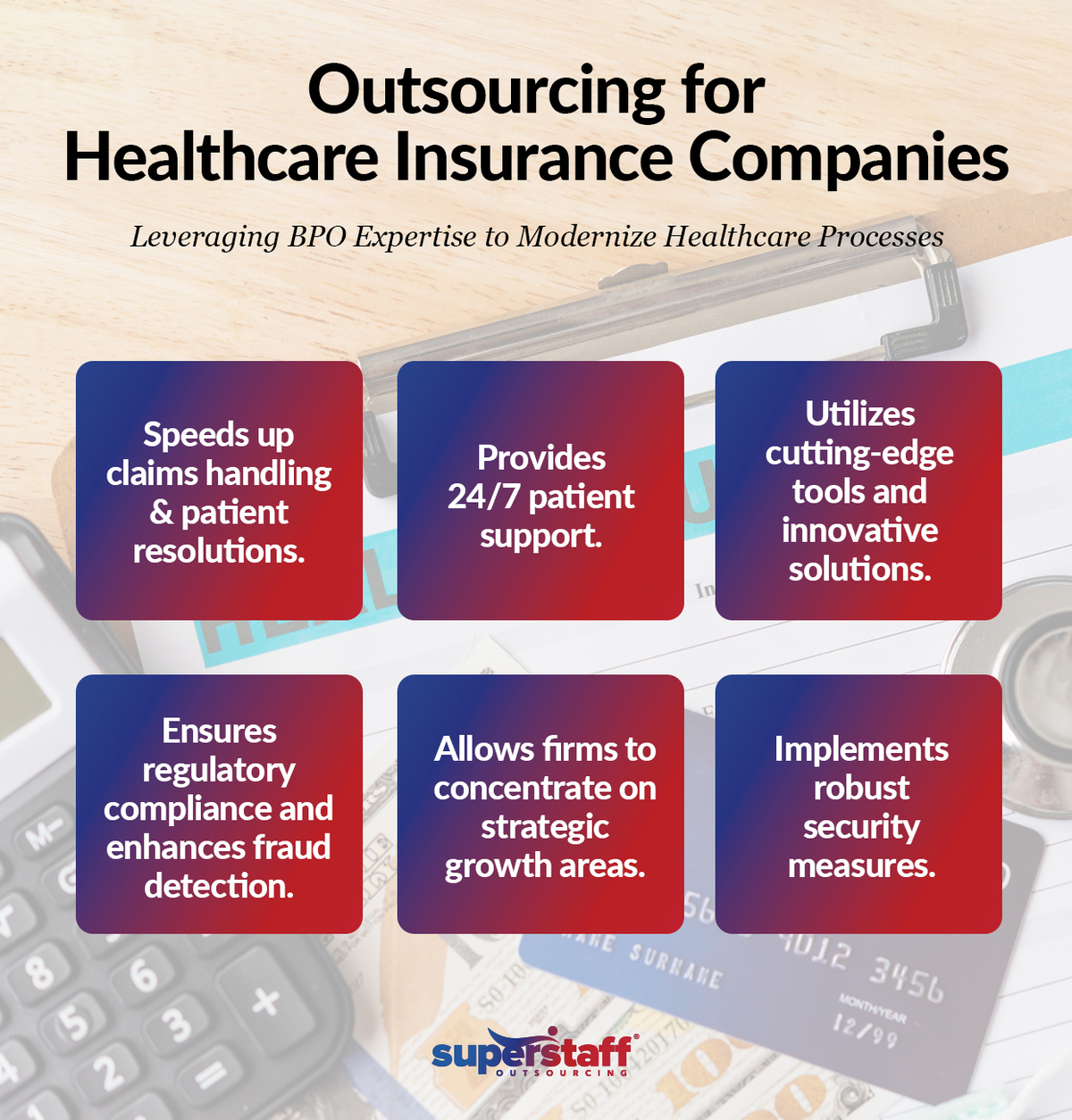
Redefine Patient-Centric Healthcare With SuperStaff
Outsourcing customer service and back-office operations isn’t just a practical move — it’s essential for elevating patient care in today’s fast-evolving healthcare insurance landscape.
At SuperStaff, we provide customized outsourcing solutions that enhance patient communication, streamline claims processing, and ensure a unified digital experience. It’s time for all stakeholders — insurance companies, healthcare providers, and policymakers — to embrace digital transformation and prioritize patient needs over bureaucracy.
Partner with us to reduce confusion, speed up claim resolutions, and deliver timely, transparent support while focusing on your core mission of providing top-notch care. Our team integrates seamlessly with your existing systems to offer consistent, efficient support, minimizing the risk of lost documents and accelerating reimbursement processes.
Transform your operations with us and join the movement toward a more efficient, responsive, and genuinely patient-centric healthcare system.